Take our patient case study quiz on axial spondyloarthritis, specially curated for you by our Editorial Panel Member, Prof. Dennis McGonagle.
A 53-year-old man (born 1969), had a low back pain at the age of 20 (1989).
Lab Tests and Diagnosis:
- HLA-B27+
- Sacroiliitis (X-ray) at the age of 29, didn’t have any extra-articular manifestations
- He was treated with non-steroidal anti-inflammatory drugs (NSAIDs) with reasonable response and was able to continue work as Taxi Driver
Coming to 2007, he was unable to work as Taxi Driver due to low back pain and stiffness and was transferred to Leeds in 2007 for second opinion.
Parameters:
- Smoker
- Basal Metabolic Rate (BMI) 27
- Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) Consistently > 7
- C-Reactive Protein (CRP) 10 mg/l
- Treated with Etanercept 50 mgs week from 2007
- X-ray at 2012 at Leeds revealed fused sacroiliac joints (SIJ)s and spine (Fig.1)
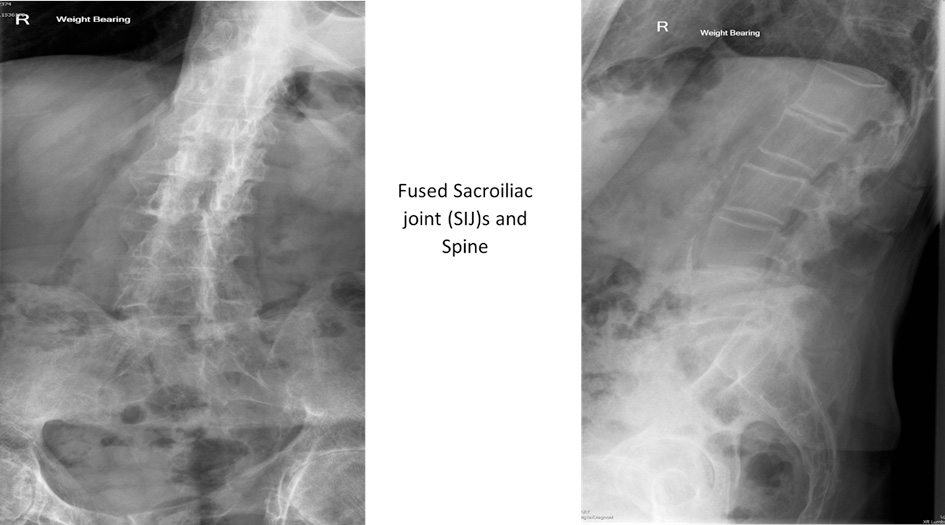
Fig.1: Fused sacroiliac joints (SIJ)s and spine
Further, there was no fusion in neck although there was neck pain and therefore Electrical muscle stimulation (EMS) was given.

Fig.2: No Fusion in Neck
In 2013, Magnetic Resonance Imaging (MRI) in Leeds showed left side sacroiliitis (circled in red) and no evidence of osteitis in the spine.

Fig.3: Left side sacroiliitis by MRI

Fig.4: Lack of Active Osteitis in Spine
As active disease was diagnosed by MRI, he was prescribed Humira 40mgs every other week (EOW) in 2013 but was discontinued due to lack of efficacy and also depression. He was then switched to Golimumab 100mgs monthly subcutaneously.
Lab Tests:
- BASDAI score always greater than 5
- CRP was normal for years
Repeat MRI following Golimumab showed resolution of bone oedema with no evidence of spinal osteitis but BASDAI score remained high.

Fig.5: Resolution of Bone Oedema
In 2018, he was switched to Secukinumab 150mgs subcutaneous regimen. He continued to smoke. CRP is normal prior to starting, BASDAI 7.5 to 5, felt somewhat better initially but was unable to return to work. In 2020, Secukinumab was stopped due to inadequate response.
Currently, he is ongoing EMS and also have constant pains, hence planning to start Upadacitinib.